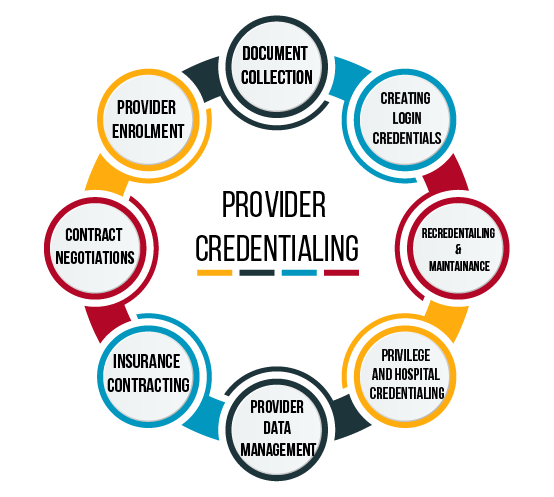
Medical credentialing is a rigorous process that verifies and assesses the qualifications, training, experience, and professional background of healthcare providers. It is essential for ensuring that healthcare professionals meet the standards set by regulatory bodies, insurance companies, hospitals, and other healthcare organizations. We assist healthcare professionals in enrolling with insurance networks, Medicare, Medicaid, and other third-party payers. Our team manages the entire enrollment process, from gathering the required documentation to submitting the application and following up on its progress. We keep track of renewal deadlines, monitors changes in regulations, and updates credentials as necessary, saving you from the administrative burden.